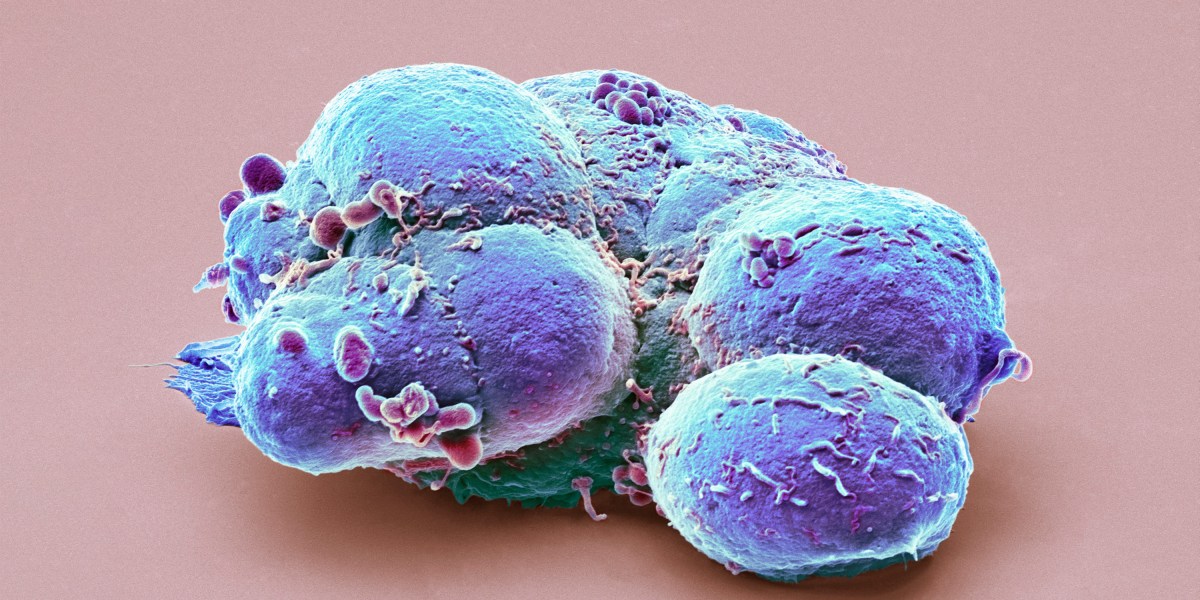
“If awards were given for the most intriguing, controversial, and hush-hush of scientific pursuits,” I wrote, “the search for the embryonic stem cell would likely sweep the categories.” It was the search for a tabula rasa cell, we told readers—one able to give rise to any other type in the human body. The embryonic stem cell was a potential “factory in a dish” that could give scientists for the first time “the ability to grow human tissue at will.” And it was taboo because the cells existed only in early-stage human embryos, which could be obtained from IVF clinics but had to be destroyed in order to isolate the cells.
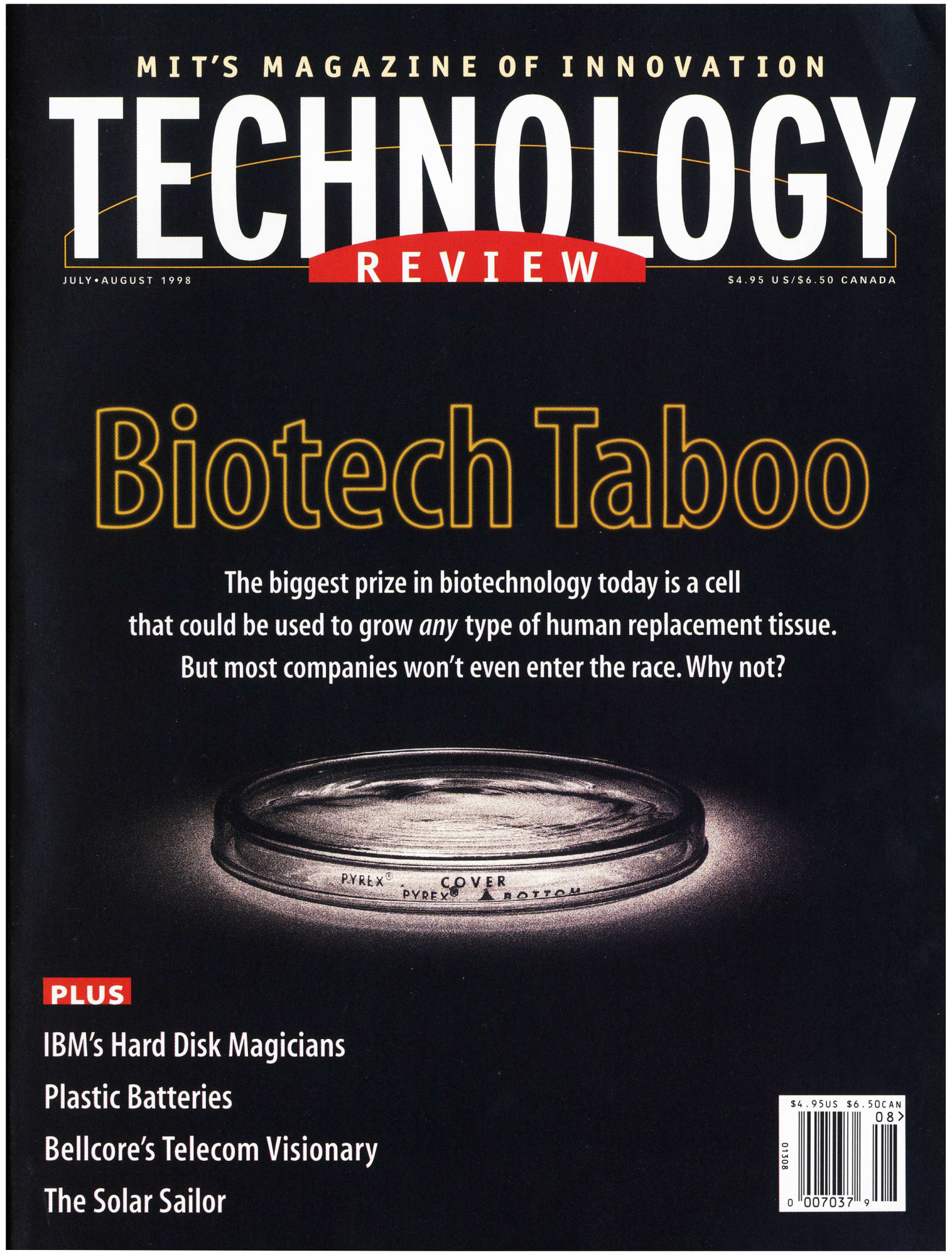
ROBERT CARDIN
A few months after our report, the scientific race reached its conclusion. That November, James Thomson at the University of Wisconsin reported he’d captured stem cells from five embryos and was keeping these cells alive, and multiplying, in his lab.
Thomson’s paper, a succinct three-pager in the journal Science, contained a sketch of how he thought stem cells would become a medical technology. Where organs or cells from cadavers are in short supply, he predicted, stem cells “will provide a potentially limitless source of cells for drug discovery and transplantation medicine,” in particular by permitting “standardized production” of specialist cell types like beating heart cells or glucose-sensing beta cells. He noted that some diseases, specifically type 1 diabetes and Parkinson’s, result from “the death or dysfunction of just one or a few cell types.” If those specific cells could be replaced, it would mean “life-long treatment.”
That vision—that the mother of all cells could replace any tissue, or even regrow organs—is what electrified a generation of researchers. “That was the closest thing to magic that I have encountered. It’s a cell that keeps dividing and makes anything. If you are a cell biologist, that is the grail,” says Jeanne Loring, a professor emerita at the Scripps Research Institute and cofounder of Aspen Neuroscience, a company that plans to treat Parkinson’s disease with a transplant of dopamine-making cells. “The problem is, how do you make them into the precise cell type that you want?” What's more, if stem cells are allowed to multiply in the lab, they can accumulate mutations, posing potential cancer risks: “That is the dark part of the magic.”
Political test
The stem-cell concept would shortly face a defining test—but it was political, not scientific. Because they’d been plucked from tiny, but living, IVF embryos, destroying them in the process, the discovery was met with outrage from the Catholic Church and other religious organizations in the US.
Two years after Thomson’s paper, George W. Bush was elected president. Now Christian conservatives had a line into the White House, and they wanted federal funding for the research on the cells blocked. Scientists, aided by patient advocates, reacted with an overwhelming lobbying campaign. Yes to cures, they rallied. “I love stem cells,” read the bumper stickers.
That equation—stem cells equals cures—made the breakthroughs seem closer than they really were. Martin Pera, editor in chief of Stem Cell Reports, an academic journal, was part of the push: in an editorial that year, for example, he wrote that treatments would be realized “soon,” if only the government and charities would fund the science. “It was all in our imagination at the time,” Pera told me when I saw him at the ISSCR meeting. “Because all we had were undifferentiated stem cells.”
Timothy Caulfield, a health law professor at the University of Alberta, would later analyze news articles and determine that scientists consistently made “authoritative statements” with “unrealistic timelines” for when cures would come. “I don’t blame the researchers,” he says. “There is a microphone in front of them, and five or 10 years is close enough yet far enough away. You have to make it exciting, revolutionary. If not, the money is going somewhere else.”
Source link